Behavioral medicine integrates biological‚ psychological‚ and social factors to understand health and disease. It focuses on preventing‚ diagnosing‚ and treating conditions through behavior-based interventions.
Definition and Scope
Behavioral medicine is an interdisciplinary field that examines the relationship between biological‚ psychological‚ and social factors in health and disease. It aims to prevent‚ diagnose‚ and treat conditions through understanding these interactions. The scope includes bio-behavioral mechanisms‚ clinical interventions‚ and public health strategies‚ integrating diverse sciences and techniques to enhance holistic well-being and achieve better patient outcomes effectively.
Importance in Modern Healthcare
Behavioral medicine plays a crucial role in modern healthcare by addressing the root causes of chronic diseases through lifestyle changes and psychological interventions. It complements traditional medical approaches by focusing on prevention and holistic wellness‚ thereby reducing healthcare costs and improving quality of life. By integrating behavioral strategies‚ it bridges the gap between mind and body‚ offering comprehensive solutions for long-term health management.

Key Concepts in Behavioral Medicine
Behavioral medicine emphasizes the biopsychosocial model‚ mind-body interactions‚ and biobehavioral mechanisms to understand health and disease‚ enabling effective prevention and treatment strategies.
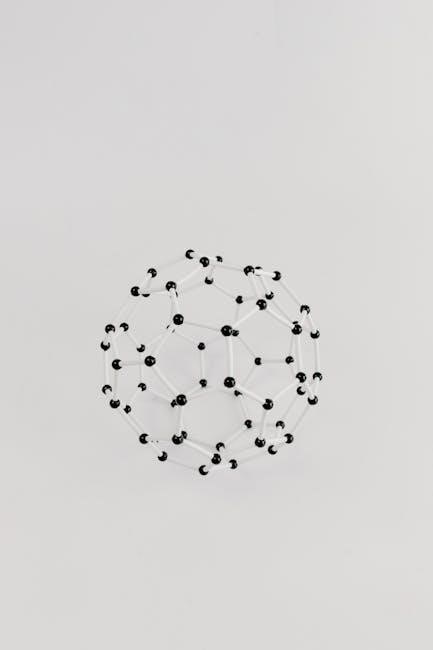
The Biopsychosocial Model
The biopsychosocial model in behavioral medicine integrates biological‚ psychological‚ and social factors to understand health and disease. It emphasizes how biological processes‚ psychological states‚ and environmental influences interact to shape well-being. This model recognizes that health outcomes are influenced by a combination of genetic predispositions‚ emotional responses‚ and social environments. By addressing these interconnected elements‚ the biopsychosocial model provides a holistic approach to diagnosis‚ treatment‚ and prevention‚ promoting comprehensive care that considers the whole person rather than isolated symptoms or conditions.
Mind-Body Interactions
Mind-body interactions are central to behavioral medicine‚ exploring how psychological states influence physical health. Stress‚ emotions‚ and behaviors affect biological processes‚ impacting susceptibility to illness and recovery. Techniques like mindfulness‚ biofeedback‚ and relaxation reduce stress‚ promoting well-being. This bidirectional relationship underscores the importance of addressing mental health in medical care‚ offering a pathway to enhance overall health outcomes through integrated approaches.
Biobehavioral Mechanisms
Biobehavioral mechanisms examine the interplay between biological systems and behavioral factors‚ such as stress‚ emotions‚ and lifestyle. These interactions influence health outcomes by affecting physiological processes like inflammation‚ immune response‚ and neuroendocrine function. For instance‚ chronic stress can trigger cardiovascular diseases by increasing blood pressure and heart rate. Understanding these mechanisms helps develop targeted interventions to modify harmful behaviors and promote health. This knowledge is crucial for preventing and managing chronic conditions‚ emphasizing the role of behavior in shaping biological health outcomes.
Clinical Diagnosis and Intervention
Clinical diagnosis in behavioral medicine involves assessing how behavioral factors contribute to medical conditions. Healthcare providers use techniques like patient interviews‚ behavioral assessments‚ and physiological measurements to identify patterns. Interventions often include behavioral therapies‚ such as cognitive-behavioral therapy (CBT)‚ biofeedback‚ and relaxation training. These methods aim to modify unhealthy behaviors and improve adherence to treatment plans. By addressing both psychological and physical aspects‚ clinical interventions in behavioral medicine promote holistic healing and better patient outcomes‚ emphasizing the interconnectedness of behavior and health.
Public Health Applications
Behavioral medicine plays a crucial role in public health by addressing lifestyle factors that contribute to chronic diseases. It emphasizes prevention through behavioral interventions‚ such as promoting physical activity‚ healthy diets‚ and stress management. Public health campaigns often incorporate behavioral strategies to encourage positive changes in populations. Policy changes‚ like taxation on sugary drinks‚ also align with behavioral medicine principles. By fostering community engagement and education‚ behavioral medicine aims to reduce health disparities and improve overall population well-being through sustainable‚ scalable interventions.

Clinical Applications of Behavioral Medicine
Behavioral medicine applies techniques like CBT‚ biofeedback‚ and mindfulness to address chronic diseases and mental health issues‚ aiming to enhance patient outcomes through holistic care.
Behavioral Interventions in Chronic Diseases
Behavioral interventions play a crucial role in managing chronic diseases by addressing lifestyle factors such as diet‚ exercise‚ and stress. Techniques like cognitive-behavioral therapy (CBT) and mindfulness meditation help patients adopt healthier habits‚ improving disease outcomes. These interventions are particularly effective in conditions like diabetes and cardiovascular diseases‚ where behavior significantly influences disease progression. By fostering sustainable lifestyle changes‚ behavioral interventions not only enhance physical health but also improve mental well-being‚ contributing to overall quality of life.
Psychological Assessments and Therapies
Psychological assessments in behavioral medicine identify mental health factors influencing physical well-being. Therapies such as cognitive-behavioral therapy (CBT) and relaxation techniques are widely used to address stress‚ anxiety‚ and depression. These interventions help patients develop coping strategies and improve emotional resilience. By integrating psychological support with medical care‚ behavioral medicine enhances overall health outcomes‚ fostering a holistic approach to treatment and prevention.

Public Health Implications
Behavioral medicine informs public health strategies by addressing lifestyle factors and promoting preventive behaviors‚ reducing chronic disease risks‚ and improving population health outcomes.
Behavioral Prevention Programs
Behavioral prevention programs focus on promoting healthy lifestyles and reducing risk factors for chronic diseases. These initiatives often include educational campaigns‚ lifestyle interventions‚ and community-based activities aimed at modifying behaviors such as diet‚ physical activity‚ and substance use. By addressing the social determinants of health‚ these programs seek to empower individuals and communities to adopt healthier habits‚ ultimately reducing the burden of preventable diseases. They are integral to public health strategies‚ emphasizing early intervention and sustainable behavior change to improve long-term health outcomes.
Policy Changes for Health Promotion
Policy changes play a crucial role in promoting health by creating environments that support healthy behaviors. Governments and organizations collaborate to implement regulations that encourage physical activity‚ healthy eating‚ and stress reduction. Examples include taxes on sugary drinks‚ smoke-free laws‚ and urban planning that promotes walking and cycling. These policies are designed to address the root causes of chronic diseases and improve public health outcomes. By integrating behavioral science into policy-making‚ societies can foster sustainable health improvements and reduce disparities in healthcare access and disease prevention.
Mental Health and Behavioral Medicine
Mental health is deeply intertwined with physical well-being‚ and behavioral medicine explores this connection. It addresses mental health conditions by integrating psychological‚ social‚ and biological factors to improve overall health outcomes through tailored interventions and therapies.
Stress‚ Anxiety‚ and Depression
Behavioral medicine addresses stress‚ anxiety‚ and depression by integrating psychological‚ social‚ and biological factors. It emphasizes the role of behavior in mental health‚ offering interventions like cognitive-behavioral therapy (CBT)‚ mindfulness‚ and relaxation techniques. Chronic stress is linked to physical health issues‚ while anxiety and depression often require holistic approaches. Behavioral interventions focus on lifestyle changes‚ coping strategies‚ and emotional regulation to mitigate symptoms and improve overall well-being. Early intervention and personalized care are critical in managing these conditions effectively.
Behavioral Interventions for Mental Health
Behavioral interventions in mental health focus on modifying harmful behaviors and thoughts through evidence-based techniques. Cognitive-behavioral therapy (CBT) is widely used to address anxiety‚ depression‚ and stress by restructuring maladaptive thought patterns. Mindfulness meditation and relaxation techniques also play a role in reducing symptoms. Behavioral activation and biofeedback are additional tools to enhance emotional regulation and coping skills. These interventions aim to empower individuals with strategies to manage mental health challenges effectively‚ promoting long-term well-being and resilience.

Chronic Diseases and Behavioral Factors
Chronic diseases like diabetes and heart disease are deeply influenced by behavioral factors such as diet‚ exercise‚ and stress management‚ highlighting the need for lifestyle interventions.
Behavioral Contributions to Diabetes
Behavioral factors play a crucial role in the development and management of diabetes. Poor dietary habits‚ sedentary lifestyles‚ and stress contribute to increased blood sugar levels. Regular physical activity and balanced nutrition are essential for maintaining glucose control. Psychological stress can exacerbate symptoms‚ while mindfulness and relaxation techniques may help mitigate these effects. Behavioral interventions‚ such as education on glucose monitoring and medication adherence‚ are vital for improving outcomes in diabetic patients. Addressing these factors can significantly reduce the risk and complications associated with diabetes.
Cardiovascular Diseases and Lifestyle
Lifestyle factors significantly influence the development and progression of cardiovascular diseases. Unhealthy behaviors‚ such as poor diet‚ physical inactivity‚ and smoking‚ increase the risk of conditions like hypertension and atherosclerosis. A balanced diet rich in fruits‚ vegetables‚ and whole grains‚ combined with regular exercise‚ can reduce these risks. Stress management techniques‚ such as mindfulness‚ also play a role in mitigating cardiovascular stress. Additionally‚ avoiding smoking and limiting alcohol consumption are critical for maintaining heart health. Addressing these lifestyle factors is essential for preventing and managing cardiovascular diseases effectively.
Pain Management in Behavioral Medicine
Behavioral medicine approaches to pain management include psychological interventions like mindfulness‚ biofeedback‚ and relaxation techniques to reduce chronic pain and improve quality of life effectively.
Chronic Pain and Behavioral Factors
Chronic pain is significantly influenced by behavioral factors‚ such as coping mechanisms‚ stress‚ and emotional responses. Psychological elements like anxiety and depression can exacerbate pain perception. Behavioral interventions‚ including cognitive-behavioral therapy (CBT)‚ mindfulness‚ and relaxation techniques‚ are effective in managing chronic pain by addressing these factors. Understanding the interplay between behavior and pain is crucial for developing personalized treatment plans that improve quality of life and reduce reliance on pharmacological treatments. This holistic approach emphasizes the role of lifestyle and mental health in pain management.
Psychological Interventions for Pain
Psychological interventions play a crucial role in managing chronic pain by addressing emotional and behavioral factors. Techniques like cognitive-behavioral therapy (CBT) help individuals modify maladaptive thoughts and behaviors associated with pain. Mindfulness-based stress reduction and relaxation exercises reduce stress and enhance coping strategies. Biofeedback and hypnosis are also effective in altering pain perception. These interventions aim to improve emotional well-being‚ reducing the emotional distress often linked to chronic pain. By integrating psychological approaches‚ patients can achieve better pain management and improved quality of life;

Substance Abuse and Behavioral Medicine
Behavioral medicine addresses substance abuse through prevention and treatment‚ focusing on psychological and behavioral interventions to reduce addiction’s impact on health and well-being.
Behavioral Approaches to Treatment
Behavioral approaches to treatment focus on modifying harmful behaviors and promoting healthier alternatives. Techniques like cognitive-behavioral therapy (CBT)‚ mindfulness‚ and biofeedback help individuals change maladaptive patterns. These methods address underlying psychological factors contributing to substance abuse‚ enabling patients to develop coping strategies and improve decision-making. By targeting the root causes of addiction‚ behavioral interventions aim to reduce relapse rates and enhance overall well-being. These evidence-based practices are integral to comprehensive treatment plans‚ offering personalized solutions for sustainable recovery.
Prevention Strategies
Prevention strategies in behavioral medicine focus on identifying and addressing risk factors before substance abuse occurs. Early interventions‚ such as educational programs and community initiatives‚ play a crucial role. Techniques like motivational interviewing and lifestyle modifications help individuals develop healthier habits. Public health campaigns and policy changes‚ such as taxation on harmful substances‚ further reduce accessibility and consumption. These strategies aim to create environments that discourage substance abuse and promote overall well-being. Community-based programs often involve collaboration with schools‚ workplaces‚ and healthcare systems to maximize reach and effectiveness.
Special Populations in Behavioral Medicine
Behavioral medicine addresses the unique needs of diverse groups‚ including children‚ adolescents‚ elderly‚ and those with severe mental illnesses‚ ensuring tailored interventions for optimal health outcomes;
Children and Adolescents
Behavioral medicine focuses on addressing the unique health needs of children and adolescents‚ integrating psychological and educational strategies to promote well-being. It targets issues like anxiety‚ behavioral disorders‚ and developmental challenges‚ emphasizing early intervention. Family and environmental factors are considered to tailor interventions‚ ensuring comprehensive care. Techniques such as CBT and biofeedback are often used to help young individuals manage stress and improve coping mechanisms. This approach highlights the importance of addressing mental and physical health early to foster long-term resilience and healthy lifestyles.
Elderly and Geriatric Care
Behavioral medicine plays a crucial role in elderly and geriatric care by addressing cognitive decline‚ chronic pain‚ and mental health issues. Interventions focus on improving quality of life through tailored therapies. Techniques such as mindfulness and relaxation help manage stress and depression. Additionally‚ behavioral strategies support adherence to treatment plans for conditions like diabetes and cardiovascular diseases. This holistic approach ensures that elderly patients receive comprehensive care that addresses both physical and psychological well-being‚ enhancing their overall health and independence.
Severe Mental Illness
Behavioral medicine addresses severe mental illnesses like schizophrenia and bipolar disorder by integrating psychological therapies with medical treatments. Cognitive-behavioral therapy (CBT) and mindfulness-based interventions help manage symptoms and improve coping strategies. These approaches focus on enhancing adherence to medication‚ reducing stigma‚ and promoting social functioning. Behavioral interventions also aim to address co-occurring physical health issues‚ such as metabolic changes‚ often associated with severe mental illnesses. This holistic approach ensures comprehensive care‚ improving both mental and physical well-being for patients with severe mental health conditions.

Future Directions in Behavioral Medicine
Future directions include personalized interventions‚ digital health tools‚ and integrating AI for predictive care. These innovations aim to enhance treatment efficacy and expand accessibility globally.
Emerging Trends
Emerging trends in behavioral medicine include the integration of digital health tools‚ such as telehealth and mobile apps‚ to enhance treatment accessibility. AI-driven predictive analytics is being leveraged to personalize interventions‚ improving outcomes. There is also a growing focus on wearable devices to monitor behavioral and physiological data in real-time. Additionally‚ advancements in behavioral genetics and epigenetics are offering new insights into how lifestyle factors influence health. These innovations are reshaping the field‚ enabling more precise and scalable interventions to address chronic diseases and mental health conditions effectively.
Research and Development
Research in behavioral medicine focuses on understanding the interplay between behavior and health. Studies explore how psychosocial factors influence chronic diseases like diabetes and cardiovascular conditions. Innovations include developing personalized interventions using AI and wearable technology. Clinical trials test the efficacy of behavioral therapies‚ such as mindfulness and biofeedback‚ in managing pain and mental health. Collaborative efforts between scientists and clinicians aim to translate findings into practical applications‚ ensuring evidence-based practices are integrated into healthcare systems worldwide‚ improving patient outcomes and promoting healthier lifestyles.
